What Does IGH Mean? Unpacking This Important Medical Term
Have you ever looked at a lab report or heard a doctor mention an acronym like "IGH" and felt a little lost? It's a rather common experience, you know, feeling a bit overwhelmed by medical language. Many people, just like those sharing their experiences in "My text," often find themselves trying to make sense of complex results, wondering what specific terms truly indicate about their health. Understanding these terms can really make a big difference, giving you a clearer picture of what's happening with your body.
Figuring out what "IGH" stands for and why it matters is, in some respects, a very good step toward feeling more in control of your health information. It’s not just about memorizing letters; it’s about grasping a piece of how your immune system works and what certain findings might point to. This particular term, IgH, often comes up in discussions about specific kinds of blood tests and conditions affecting your immune system, as we see from questions people ask about MGUS or myeloma in "My text."
This article aims to shed some light on what IGH actually means, why it’s a topic of interest in medical conversations, and what its presence or particular characteristics might suggest. We'll explore its role in the body and how it connects to various health situations, providing a clearer view for anyone looking to better understand their own or a loved one's medical journey. So, let's take a look at this important part of our body's defense system.
- How Old Is North West
- Whistle Express Car Wash
- Dairy Queen Grill Chill
- Jojo Siwa Magazine Cover
- Green Tea Shot Recipe
Table of Contents
- What is IGH? A Basic Introduction
- The IGH Gene and Our Immune System Defenders
- IGH in the Context of B Cells and Antibodies
- When IGH Becomes a Focus in Medical Discussions
- How IGH is Investigated: Medical Tests
- Making Sense of IGH Test Results
- Why Knowing About IGH Can Help You
- Frequently Asked Questions About IGH
- A Final Thought on IGH
What is IGH? A Basic Introduction
So, what exactly does IGH mean? Well, IgH stands for Immunoglobulin Heavy Chain. To put it simply, it’s a very important component of antibodies, which are proteins your immune system makes to fight off things that could make you sick, like viruses and bacteria. You know, these little defenders are pretty amazing, and IgH is a big part of how they work.
Imagine your body's immune system as a highly trained army, and antibodies are its specialized weapons. Each antibody has a specific target, and the heavy chain, or IgH, helps determine that target and the antibody's overall shape. It's almost like the main body of the weapon, which then gets specialized parts attached to it. Without a proper IgH, these antibodies just wouldn't be able to do their job effectively, which is quite a big deal for keeping us healthy, you know.
This heavy chain is encoded by a set of genes, and these genes have a rather clever way of rearranging themselves to create a huge variety of antibodies. This variety is actually what allows your immune system to recognize and respond to countless different threats. It’s a truly fascinating bit of biological engineering, enabling our bodies to adapt to new challenges constantly.
- Cronología De Inter Milan Contra Fc Barcelona
- Missouri Star Quilt Company
- How Tall Is Benson Boone
- Bbq Chicken Urban Dictionary
- Victoria Secret Credit Card
The IGH Gene and Our Immune System Defenders
The instructions for making the immunoglobulin heavy chain are found in a specific part of our DNA, called the IGH gene locus. This gene area is located on chromosome 14 in humans, and it's rather complex, with many different segments. These segments, you see, can combine in various ways, a process known as V(D)J recombination. This recombination is a bit like having a LEGO set where you can create countless different structures from the same basic bricks.
This gene rearrangement is absolutely essential for creating the incredible diversity of antibodies that our bodies need. Think about it: every time you encounter a new germ, your immune system needs to be able to make a custom-fit antibody to neutralize it. The IGH gene, with its ability to shuffle and combine its parts, is what makes this customization possible. It's a truly remarkable system that allows for a vast repertoire of immune responses.
The uniqueness of these rearrangements is also why the IGH gene is often studied in certain medical situations. Because each B cell (a type of white blood cell that makes antibodies) creates its own unique IGH rearrangement, detecting a specific, identical rearrangement can sometimes point to an abnormal growth of B cells. This can be a very important clue for doctors when they are looking into certain conditions, as a matter of fact.
IGH in the Context of B Cells and Antibodies
B cells are the primary producers of antibodies in your body. Each B cell, when it's just starting out, goes through this process of IGH gene rearrangement to create a unique heavy chain for the antibody it will eventually produce. This heavy chain then combines with a light chain to form a complete antibody molecule. It's a bit like assembling a complex machine where each part has to fit just right.
When a B cell encounters something it recognizes, like a virus, it gets activated and starts making many copies of itself. These copies, or plasma cells, then pump out large amounts of the specific antibody. The IGH part of these antibodies is crucial for their function, helping them to bind to and neutralize the invaders. So, really, the IGH is central to this whole protective process.
The variety in the IGH gene allows for a vast array of antibody specificities, meaning your immune system can recognize a huge number of different threats. This adaptability is what keeps us safe from a constantly changing world of pathogens. Without this intricate system, our bodies would be much less equipped to handle infections and illnesses, which is quite a serious thought.
When IGH Becomes a Focus in Medical Discussions
While IGH is a normal and vital part of our immune system, it becomes a topic of particular interest in medicine when there are concerns about certain blood disorders or cancers. In these situations, the normal, diverse production of antibodies can sometimes go awry. Doctors might look at IGH patterns to help diagnose or monitor conditions that involve B cells or plasma cells. This is where "My text" really comes into play, as people discuss their test results and what they mean for conditions like MGUS or myeloma, you know.
For instance, if all the B cells in a person's body were producing antibodies with the exact same IGH heavy chain, that would be quite unusual. Normally, you'd expect a wide range of different IGH types, reflecting a healthy, diverse immune response. So, when something looks too uniform, it can signal a problem. This is a very key concept in understanding some blood test results.
The questions raised in "My text" about "small signs of myeloma" or whether "the amount is so low its hard to detect" directly relate to these kinds of investigations. When a doctor investigates IgH, they're often trying to figure out if the B cells or plasma cells are behaving normally or if there's an uncontrolled growth of a single type of cell. It’s a very important diagnostic tool, actually.
Monoclonal Versus Polyclonal IGH Patterns
One of the most important distinctions when discussing IGH in a medical context is between "monoclonal" and "polyclonal" patterns. A "polyclonal" pattern means that there are many different types of B cells, each making a slightly different version of the IgH heavy chain. This is the normal, healthy state, indicating a diverse and responsive immune system. As someone in "My text" mentions, "The remaining sig + b cells are polyclonal," which is usually a good sign, showing variety.
On the other hand, a "monoclonal" pattern suggests that a single B cell has multiplied uncontrollably, creating a large number of identical copies. All these copies then produce antibodies with the exact same IGH heavy chain. This lack of diversity can be a red flag, as it might indicate the presence of a blood cancer, like myeloma, or a pre-cancerous condition, such as MGUS. It’s a very significant difference, really, in what these patterns suggest.
Detecting a monoclonal IGH rearrangement is often a key step in diagnosing these conditions. It helps doctors pinpoint the abnormal cell population and understand its characteristics. This distinction is, arguably, one of the most fundamental pieces of information gained from IGH testing. It helps guide further investigation and potential treatment options, so it's quite critical.
IGH and MGUS (Monoclonal Gammopathy of Undetermined Significance)
MGUS, or Monoclonal Gammopathy of Undetermined Significance, is a condition where plasma cells produce a monoclonal protein, but it doesn't meet the criteria for multiple myeloma or other related disorders. Someone in "My text" mentions, "I have been diagnosed with mgus since 2003," showing how common this diagnosis can be. In MGUS, there's an abnormal clone of plasma cells, all making the same immunoglobulin, which includes a specific IGH. The "monoclonal" aspect here is very important.
While MGUS itself often causes no symptoms and might not require immediate treatment, it's considered a pre-cancerous condition. This means there's a slightly increased chance that it could progress to a more serious condition like multiple myeloma over time. Monitoring the levels of this monoclonal protein, which is often tied to the IGH, is a key part of managing MGUS. So, understanding the IGH connection helps people grasp why they are being watched so closely.
The question from "My text" – "does it mean i don't have a mgus, or just the amount is so low its hard to detect" – highlights the nuances of diagnosis. Sometimes, the amount of monoclonal protein is very low, making detection a bit challenging, but its presence, even in small amounts, can still be significant for monitoring purposes. It’s a rather delicate balance doctors consider.
IGH in Myeloma and Other Blood Conditions
Multiple myeloma is a cancer of the plasma cells, which are B cells that have matured to produce antibodies. In myeloma, a single, abnormal clone of plasma cells grows out of control in the bone marrow, producing a large amount of a specific monoclonal immunoglobulin. This abnormal immunoglobulin, with its unique IGH, is what causes many of the problems associated with myeloma. The discussion in "My text" about "small signs of myeloma" or "mrd negative" directly relates to this.
The IGH gene rearrangement in myeloma cells is usually unique to that specific cancer. This makes it a very useful marker for diagnosis and for tracking the disease. For instance, if doctors can identify the specific IGH rearrangement in a patient's myeloma cells, they can then use highly sensitive tests to look for even tiny amounts of these cells in the blood or bone marrow, a process often called minimal residual disease (MRD) testing. This is what the question about "mrd negative" in "My text" is getting at.
IGH rearrangements are also relevant in other B-cell lymphomas, where similar clonal expansions occur. Identifying these specific genetic changes helps doctors classify the type of lymphoma and choose the most effective treatment. It's a truly powerful piece of information for personalizing care, as a matter of fact. You can learn more about various blood cancers and their characteristics from reputable health organizations.
How IGH is Investigated: Medical Tests
When doctors need to investigate IGH, they use several specialized tests to look for specific patterns or rearrangements in the genes. These tests are designed to detect if there's a monoclonal population of B cells or plasma cells, or if there are specific genetic changes that are known to be associated with certain conditions. The mention of a "fish probe" in "My text" points directly to one of these important diagnostic tools.
These tests are often performed on samples of blood or bone marrow, as these are the places where B cells and plasma cells are found in significant numbers. The goal is to get a very clear picture of what the IGH genes look like in these cells. This helps doctors make an accurate diagnosis and understand the specific characteristics of a patient's condition, which is quite vital for planning care.
The precision of these tests has really improved over the years, allowing for earlier and more accurate detection of abnormalities. This means that conditions like MGUS or early myeloma can be identified sooner, potentially leading to better outcomes for patients. It's a very encouraging development in medical diagnostics, truly.
FISH Probes and IGH Rearrangements
Fluorescence In Situ Hybridization, or FISH, is a powerful technique often used to detect chromosomal abnormalities, including those involving the IGH gene. As someone in "My text" asks, "Can somebody help me with understanding the results of the fish probe i had done on my biopsy in november," it’s clear this test is a common part of the diagnostic process for many.
With FISH, scientists use fluorescent "probes" that are designed to stick to specific parts of chromosomes, including the region where the IGH gene is located. If there's a rearrangement, like a translocation where a piece of chromosome 14 (containing IGH) breaks off and attaches to another chromosome, the FISH probe can light up in an unusual pattern. This gives doctors a visual clue about genetic changes within the cells.
These IGH translocations are particularly important in conditions like multiple myeloma and some lymphomas, as they can influence how aggressive the disease is and how it might respond to treatment. So, a FISH probe can give very specific and actionable information. It's a truly advanced way of looking at our genetic material.
Other Methods for Looking at IGH
Besides FISH, other molecular tests can also be used to analyze IGH gene rearrangements. Polymerase Chain Reaction, or PCR, is another common method. PCR can detect very small numbers of cells with a specific IGH rearrangement, making it incredibly sensitive for finding minimal residual disease (MRD) after treatment. This is very relevant to the question in "My text" about "mrd negative" results.
Next-generation sequencing (NGS) is also becoming increasingly important. This technology can read the DNA sequence of the IGH gene with great detail, identifying specific mutations or unique rearrangements that might not be picked up by other methods. NGS provides a very comprehensive look at the IGH gene, offering a wealth of information for diagnosis and personalized treatment planning.
These various testing methods, each with its own strengths, provide doctors with a robust toolkit for understanding the IGH status in a patient's cells. The choice of test often depends on the specific clinical question and the suspected condition. So, you know, there are many ways to get to the bottom of things.
Making Sense of IGH Test Results
Getting test results that mention IGH can be a bit unsettling, especially when you're not entirely sure what the terms mean. As someone in "My text" asks, "From what i understand these numbers aren't very high, but i don't know what to make of this, does it mean i don't have a mgus, or just the amount is so low its hard to detect," it's clear that interpreting these results requires careful explanation.
Generally, if a test indicates a "polyclonal" IGH pattern, that's typically a good sign, suggesting a healthy and diverse immune system. If a "monoclonal" IGH rearrangement is detected, it means there's a single, abnormal clone of B cells or plasma cells. The presence of such a clone might lead to a diagnosis of MGUS, multiple myeloma, or another related condition, depending on other clinical findings. It’s a very important distinction, truly.
The specific characteristics of the IGH rearrangement, such as the type of translocation found by FISH, can also give clues about the likely behavior of the disease and how it might respond to different treatments, like Revlimid, which is mentioned in "My text." These details help doctors tailor treatment plans to each individual, which is pretty amazing. Learn more about specific diagnostic tests on our site.
Why Knowing About IGH Can Help You
Understanding terms like IGH, even just the basics, can really empower you as a patient or caregiver. When you have a general grasp of what your doctors are discussing, you can ask more informed questions, participate more fully in decisions about your care, and feel less anxious about the unknown. It's a very human need, to understand what's happening to you.
For example, if you know that a monoclonal IGH rearrangement is linked to MGUS or myeloma, you can better appreciate why your doctor might recommend regular monitoring, even if you feel perfectly well. It helps you see the bigger picture and why certain tests or follow-up appointments are necessary. This kind of knowledge helps you be a more active partner in your health journey.
Ultimately, knowing what IGH means helps demystify some of the complex medical jargon, turning confusing terms into understandable pieces of information. This clarity can make a significant difference in how you approach your health and communicate with your medical team, which is quite a valuable thing.
Frequently Asked Questions About IGH
Here are some common questions people often have about IGH:
What is the main function of IGH in the body?
Basically, IGH, or Immunoglobulin Heavy Chain, is a crucial part of antibodies. Antibodies are proteins our immune system makes to find and neutralize things that can make us sick, like bacteria and viruses. The heavy chain helps give the antibody its specific shape and determines its overall class, so it's very important for our body's defense.
Why would a doctor order a test for IGH rearrangements?
A doctor might order an IGH rearrangement test if they suspect a condition involving abnormal B cells or plasma cells, such as MGUS, multiple myeloma, or certain types of lymphoma. Detecting a specific, identical IGH rearrangement can indicate that a single abnormal cell has multiplied, which is a key sign of these conditions. It helps with diagnosis and understanding the specific nature of the disease, you know.
Does an IGH rearrangement always mean I have cancer?
Not necessarily. While an IGH rearrangement can be a sign of cancer like multiple myeloma or lymphoma, it can also be found in conditions like MGUS (Monoclonal Gammopathy of Undetermined Significance), which is a pre-cancerous state that might not progress to cancer. The meaning of an IGH rearrangement always needs to be considered alongside other test results and clinical findings by your doctor. It's a piece of the puzzle, not the whole picture, as a matter of fact.
A Final Thought on IGH
Understanding what IGH means is a step towards better health literacy. It helps bridge the gap between complex medical science and your personal health journey. Remember, while this article provides general information, your specific medical situation is unique, and discussing your results with your healthcare provider is always the best approach. They can give you the most accurate and personal advice based on your individual circumstances, which is truly what matters most.
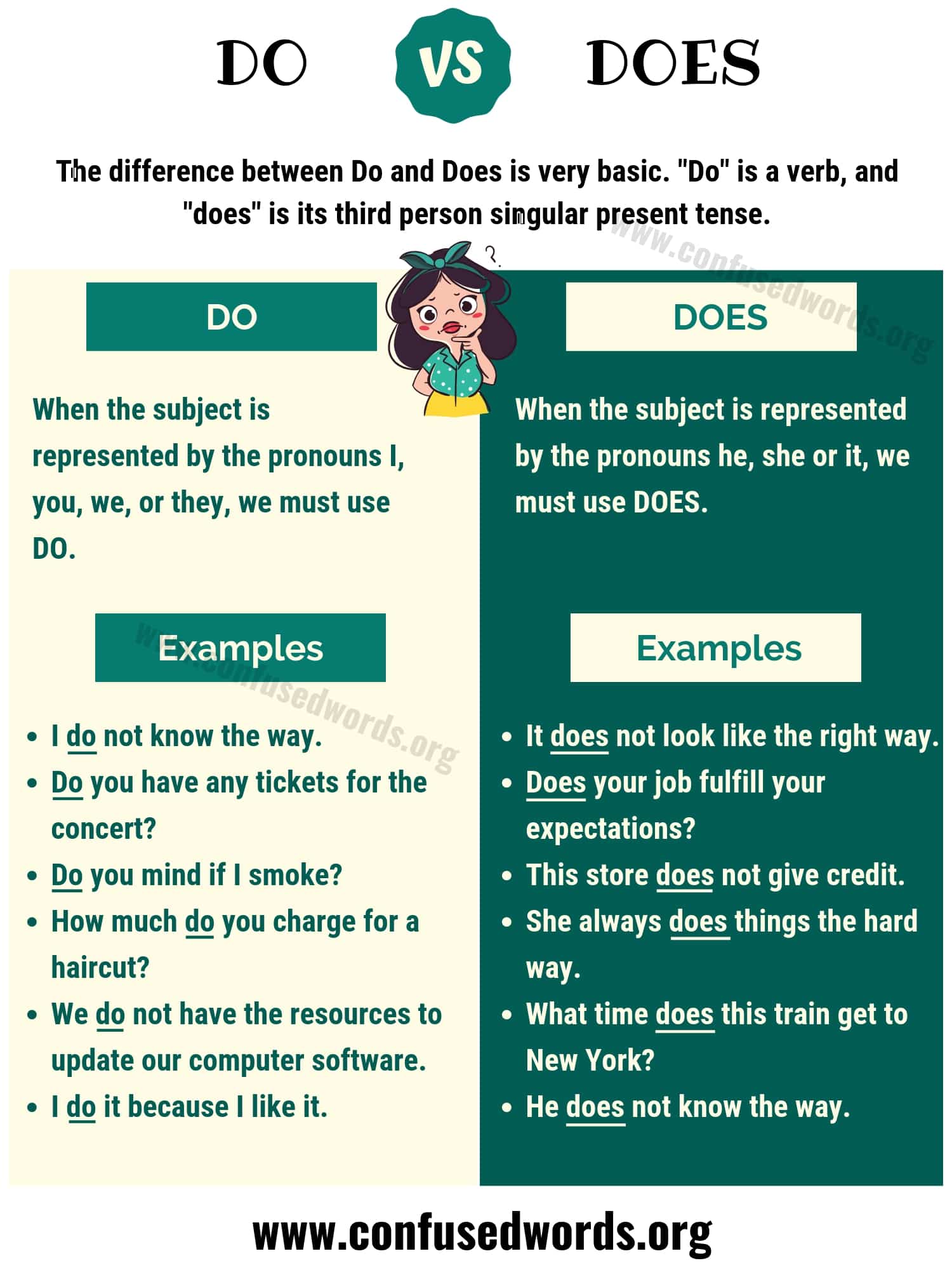
Do vs. Does: How to Use Does vs Do in Sentences - Confused Words
Do vs Does Questions in the Present Simple Tense | Learn English
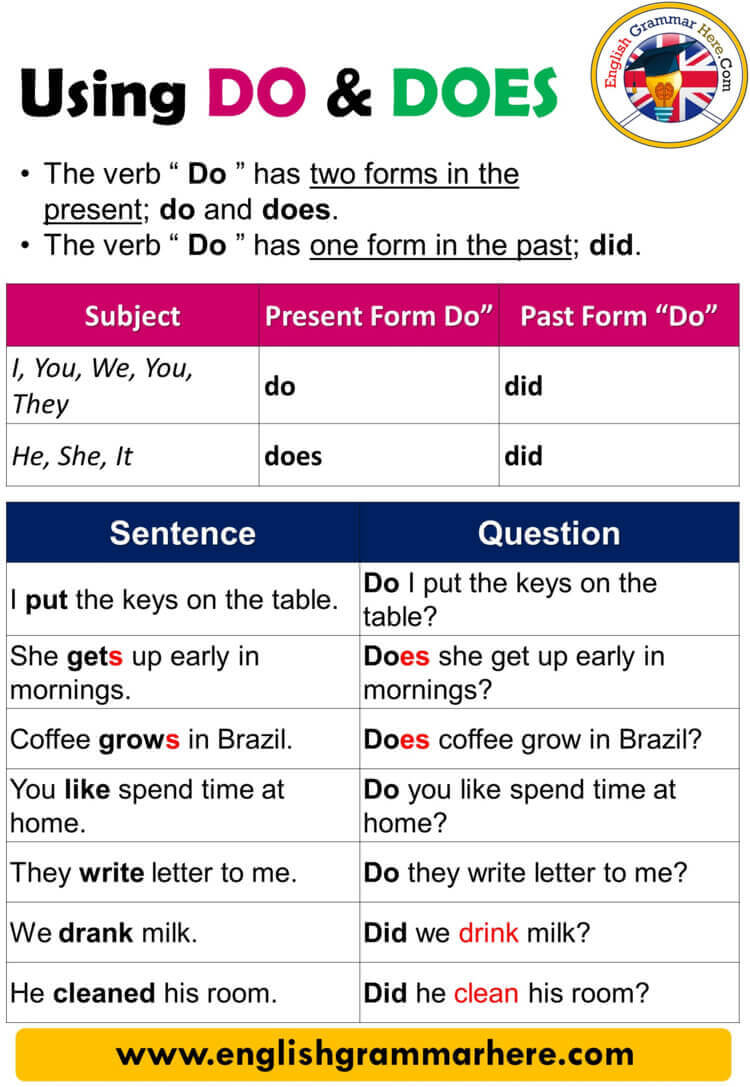
Using Do and Does, Definition and Example Sentences - English Grammar Here